Several high-profile cases have highlighted the limitations of traditional mammograms in detecting breast cancer in dense breast tissue. These cases brought breast density and its significance to the forefront of the discussion of mammography, breast imaging and women’s health overall.
The following article draws upon our conversation with Miranda Melton, RT(R)(M), Director of Women’s Imaging education at MTMI. She holds years of experience as a radiologic technologist and mammographer in the state of Missouri and now oversees courses and events related to Women’s Imaging. With a fervent passion for women’s health education, Melton instructs multiple workshops and programs with MTMI.
Why Is Breast Density a Hot Topic?
About two decades ago, several women including Executive Director of DenseBreast-Info, JoAnn Pushkin, were diagnosed with late-stage breast cancer despite having regular annual mammograms. “One year they get told everything's fine, and then the very next year they've got stage three breast cancer,” Melton says.
When pathologists examined their breast tissue, they found that the cancer had likely been present for several years but was not detected in previous mammograms due to the density of the breast tissue. Dense breast tissue can mask tumors, making them difficult to spot with standard mammograms. The cancer in these cases only became visible once it had grown large enough to alter the tissue pattern, prompting further examination with an ultrasound.
The women questioned why their dense breast tissue was not flagged earlier and why additional screening methods like ultrasounds were not suggested. They learned that had they undergone an ultrasound the previous year, the cancer might have been detected earlier, potentially sparing them from more aggressive treatments and improving their prognosis.
Their inquiries revealed that many providers had not been informing patients about their breast density or the benefits of supplemental screenings like ultrasounds. The traditional approach had been to rely solely on mammograms, partly because ultrasounds were not approved for routine screening and often not covered by insurance.
New FDA Breast Density Requirement (MQSA)
The above cases sparked a movement for greater transparency and patient education regarding breast density. The women argued that if they had known about their dense breast tissue and the potential benefits of additional screening, they would have requested it (even at personal expense) to detect cancer earlier. This push for change has led to increased awareness and legislative efforts to ensure that patients are informed about their breast density and the associated risks.
Changes in Reporting Requirements
Changes to breast density reporting requirements under the FDA's Mammography Quality Standards Act (MQSA) were initiated by a small group of women advocating for greater transparency. These advocates successfully convinced the state of New Jersey to require that women be notified about their breast density, setting a precedent that other states followed. Over time, 38 states adopted similar requirements, though each state's approach varied. Some states mandated detailed notifications about the specific type of breast density, recognizing the implications for cancer detection, while others provided more general notifications, leaving detailed discussions to the patient's healthcare provider.
Breast imaging centers were required to comply with their state's laws, with the option to exceed these requirements if desired. The growing state-level adoption prompted the FDA to standardize breast density reporting language across all states to ensure consistency.
Federal Regulations
In 2019, the FDA announced plans to create uniform breast density notification language for all 50 states. However, the onset of the COVID-19 pandemic in 2020 delayed these efforts. With the pandemic subsiding, the FDA revisited the initiative and released the standardized language, giving states time to prepare for the transition. By September 2024 the mammography report must include an overall assessment of breast density, classified in one of the following categories:
- "The breasts are almost entirely fatty."
- "There are scattered areas of fibroglandular density."
- "The breasts are heterogeneously dense, which may obscure small masses."
- "The breasts are extremely dense, which lowers the sensitivity of mammography."
In addition, patient lay summaries must include one of the following notification statements:
- "Breast tissue can be either dense or not dense. Dense tissue makes it harder to find breast cancer on a mammogram and also raises the risk of developing breast cancer. Your breast tissue is not dense. Talk to your healthcare provider about breast density, risks for breast cancer, and your individual situation."
- "Breast tissue can be either dense or not dense. Dense tissue makes it harder to find breast cancer on a mammogram and also raises the risk of developing breast cancer. Your breast tissue is dense. In some people with dense tissue, other imaging tests in addition to a mammogram may help find cancers. Talk to your healthcare provider about breast density, risks for breast cancer, and your individual situation."
For states with existing breast density notification laws, the process requires an additional step. These states must rescind their current laws so facilities can replace it with the FDA language. This requirement ensures a uniform transition.
The FDA has set a deadline of September 10, 2024, for this transition. While states were aware of this timeline and working toward compliance, change timelines might be different for each state. States with existing notification requirements must continue using their current language in addition to the FDA language until the rescind is final.
Line Between Technologist vs. Physician
Mammography technologists cannot independently discuss breast density findings and their implications directly with patients. This information must be interpreted and communicated by a radiologist. The mammography technologist's role is to perform the mammogram and provide the images to the radiologist, who then evaluates the breast density and includes this information in a report.
Although technologists can identify whether breast tissue appears fatty or dense and understand the four categories of breast density, the precise categorization and its clinical implications must come from a physician. The decision between the different categories—such as distinguishing between the two fatty categories (A or B) or the two dense categories (C or D)— will be made by the interpreting physician. Historically, categorizing breast tissue has been done by an actual radiologist. Now, however, artificial intelligence has a place in the mammography realm because it can continually learn and improve the accuracy of its results based on the volume of mammograms it examines. Automated software programs built into radiology systems can help yield more consistent results with mammographic reporting.
In imaging centers that offer same-day results, the mammography technologist will perform the mammogram and then have the patient wait while the images are reviewed by the radiologist. The radiologist provides the results to the technologist, who then communicates these findings to the patient, perhaps accompanied by a detailed report and additional resources such as pamphlets or websites for further information. This process ensures that the information given to the patient is accurate and interpreted by a qualified physician.
1. What Are Dense Breasts?
Dense breasts are characterized by having a higher proportion of fibroglanduar tissue compared to fatty tissue. To help visualize this, think of the breast tissue as a combination of rubber bands and grapes. The rubber bands represent the fibrous (fibro) tissue, and the grapes represent the glandular tissue. In a dense breast, there are more "grapes" (glandular tissue) held together by "rubber bands" (fibrous tissue), filling up more of the breast.
Typically, an average breast consists of about 50% fatty tissue and 50% fibroglandular tissue, with an average thickness of about 4.2 centimeters. However, the size of the breast does not necessarily correlate with its density. A person with small breasts can still have dense breasts if they have a higher proportion of glandular and fibrous tissue. Similarly, someone with larger breasts can have less density if their breasts contain more fatty tissue. Dense breasts can vary significantly in size and shape, but the key factor is the relative amount of fibroglandular tissue present versus the amount of fatty tissue present.
2. What Causes Dense Breast Tissue?
Dense breast tissue is primarily influenced by female hormones, such as estrogen and progesterone. This development begins during gestation, where some hormonal influence is received from the mother. Significant changes in breast tissue occur during puberty when these hormones activate, stimulating the growth of glandular tissue.
The amount of dense tissue a person has is determined by their unique hormonal and genetic makeup, which varies from individual to individual.
3. Does It Increase Cancer Risk?
Dense breast tissue does increase cancer risk. There are two main types of breast cancer: ductal cancer, which occurs in the ducts (stems), and lobular cancer, which occurs in the lobules (grapes). The more glandular tissue (grapes) someone has, the greater the opportunity for cancer to develop, as there are more spaces for it to grow.
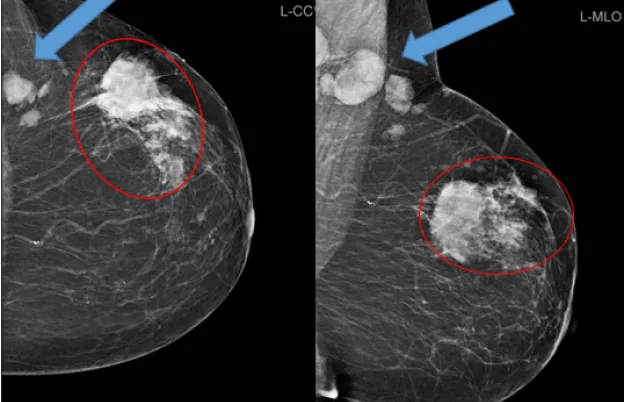
Breast cancers often grow due to hormonal influences, as hormones stimulate the growth of breast tissue and can also promote the development and growth of cancer. Dense breasts not only increase the risk of developing breast cancer but also make it harder to detect on mammograms. Denser tissue can conceal cancers because both dense tissue and cancer appear white on mammograms, making them difficult to distinguish from one another.
If you imagine a large bowl with a handful of grapes, it is easy to spot a few blueberries or raspberries among them. But, as Melton explains, “If you have a bowl full of grapes, and in the middle somewhere there are some blueberries or raspberries, you really wouldn't see them.”
4. Can Breast Density Change?
Breast density can indeed change over time, primarily due to hormonal fluctuations. When a woman goes through menopause, the decline in hormone levels causes the fibroglandular tissue in the breast to diminish and be replaced by fat.
However, if a woman takes hormone replacement therapy (HRT) during menopause, it can increase breast density again, as the hormones stimulate the growth of glandular tissue. This principle applies to men as well. If a man takes estrogen, it can lead to the growth of breast tissue, thereby increasing his risk of developing breast cancer.
Therefore, hormonal changes—whether due to natural processes like menopause or medical interventions like HRT—play a significant role in altering breast density and associated cancer risks. In addition, the longer you have had hormones, the higher your risk. If a woman has early onset of menarche (before age 12) and late onset of menopause (after age 55), she has had a longer lifetime exposure. Additionally, if she has never had pregnancies, has never breastfed, she will have denser breast tissue and consequently a higher risk of developing cancer.
5. How Is Breast Density Measured?
Breast density is measured by looking at an image of the breast using mammography. If you need to look beyond that density, you might use other screening modalities (discussed further below).
Categories A, B, C, D
Breast density is categorized into four groups (categories A through D) based on the amount of fibroglandular tissue present:
- Category A (almost entirely fatty): Breasts with few glandular clusters and less than 25% dense tissue. This category has the lowest risk of developing breast cancer, although the risk is not eliminated.
- Category B (scattered areas of fibroglandular density): 25% to 50% of dense tissue and the rest being fat.
- Category C (heterogeneously dense): 51% to 75% dense tissue with the remainder being fat. In this category, the dense tissue can start to obscure small masses, making it harder to detect cancer.
- Category D (extremely dense): More than 75% dense tissue and less than 25% fat. This category significantly lowers the sensitivity of mammograms, making cancer detection more difficult. Women in this category have a three to four times higher likelihood of developing breast cancer compared to those in Category A.
In the United States, approximately 50% of women fall into the C and D categories, indicating higher breast density, while the other 50% are in the A and B categories.
6. Is Additional Screening Recommended or Required?
When a woman is categorized as having heterogeneously dense (Category C) or extremely dense (Category D) breasts, additional screening is often recommended. For these categories, ultrasound is typically suggested to provide a more comprehensive evaluation. If the woman has other risk factors that place her in a high-risk category, an MRI may also be recommended for screening. These additional breast imaging methods help improve the detection of breast cancer in dense breast tissue, where mammograms alone may not be as effective.
7. What Is the Best Screening for Dense Breasts?
3D Mammography
Also known as digital breast tomosynthesis, 3D mammography is becoming the standard of care across the U.S., though not all facilities have this capability yet. While everyone has access to digital (2D) mammography—which is already a significant improvement over the film screen method—3D mammography offers enhanced detection, especially for dense breast tissue.
3D mammography works by taking multiple images of the breast from different angles, allowing the radiologist to examine the breast layer by layer. This separation of tissue layers provides a clearer view and a better chance of detecting hidden or cancers. Therefore, while getting any mammogram is essential, a 3D mammogram is particularly beneficial for those with dense breasts as it increases the likelihood of early cancer detection.
Breast Density and Screening Ultrasound
Mammography is often combined with Breast Ultrasound to evaluate breast tissue. Ultrasound can also be used as a primary screening tool for those with dense breasts. Breast Ultrasounds are done in two ways:
- Automated: Automated breast ultrasounds are used by some facilities, in which a machine performs a scan of the breast divided into four quadrants (two on top, two on bottom) and automatically generates results.
- Handheld: Ultrasound breast imaging is performed with a handheld probe to examine the specific area(s) of interest.
MRI for Dense Breast Screening
MRI can serve as a breast imaging screening tool. This is not to say that MRI is a “better” modality compared to mammograms and ultrasounds; all three have their own set of pros and cons.
8. How Should You Respond to Patient Questions About Breast Density?
When patients ask about breast density, it is important to provide clear and consistent information based on your facility's guidelines, which are usually determined by the lead interpreting physician or radiologist. This way, you provide the patient with a solid understanding of their breast density, the implications for their health, and the recommended next steps for further screening and consultation with their healthcare provider.
Here is a structured approach to addressing these questions:
- If patients request information on dense breasts, provide educational materials. Give the patient a pamphlet or direct them to resources like DenseBreast-info, Inc. | Dense Breast Tissue Information Resource or the American College of Radiology website for more information and next steps about dense breast tissue.
- Refer to their primary care provider. Emphasize the importance of discussing the findings and recommendations with their primary care doctor or OB-GYN. You could say, "We will send all the details to your doctor. Please have a deep conversation with them about your next steps."
- Use specific language. Ensure the patient understands the terminology used in their report. For instance, "Your report will indicate if your breasts are heterogeneously dense, which may obscure small masses, or if they are extremely dense, which lowers the sensitivity of mammography."
- Follow facility protocol. Always follow the guidelines set by your facility and ensure you direct the patient back to their provider for results.
9. Why Is Breast Density Important?
From the patient's perspective, understanding breast density is essential for making informed decisions about their health. Even though dense breast tissue can make mammography less effective, it underscores the importance of never missing an annual mammogram.
From a technologist's perspective, patients need to understand what’s happening inside their bodies. Someone knowing they have dense breast tissue empowers them with knowledge about their health. Dense breast tissue isn’t a problem itself, but it can increase the risk of breast cancer and make it harder to detect.
Using a risk assessment that includes medical history and breast density can help determine the overall risk of developing breast cancer. Knowing this information helps patients and doctors decide whether additional screening tools, like ultrasound or MRI, are needed.
It’s also essential to recognize that many women diagnosed with breast cancer do not have a family history of the disease; 85% of breast cancers occur in women with no family history. Thus, understanding one’s breast density is a key part of managing breast health. Dense breast tissue is one of the risks, and being aware of it can help patients take proactive steps in their healthcare.
“Only 15% of the cancers we diagnose come from women who've had it in their family,” Melton emphasizes. “So, somebody has to be the first, and that person could be you.”
10. Can You Reduce Breast Density?
Unfortunately, having dense breasts is something you inherit and cannot alter significantly. While avoiding hormone replacement therapy can prevent an increase in density, HRT may still be recommended for some women.
A doctor might recommend HRT as a temporary solution to alleviate menopausal symptoms, even if you have dense breast tissue. If you have no other risk factors, HRT could be appropriate for you. Once you stop taking hormone therapy and time passes, your breast density will decrease naturally. However, it’s important to discuss any concerns with your healthcare provider to make informed decisions about your treatment and breast health.
11. What Should a Patient Do If Their Mammogram Report Shows Dense Breast Tissue?
When a mammogram report shows dense breast tissue, patients must discuss the findings with their doctors. Ensuring that their primary care physician or OB-GYN understands the significance of dense breast tissue is important, as they often focus on overall health rather than just breast health.
Radiology departments are increasingly recognizing the need to educate primary care physicians and OB-GYNs about the implications of dense breast tissue. This education helps ensure that doctors can provide informed guidance to their patients. If a report indicates dense breast tissue, a doctor might recommend additional tests such as an ultrasound or MRI to get a clearer view.
Therefore, patients should actively engage with their healthcare providers to understand their breast density and discuss any necessary follow-up tests or screenings. This proactive approach can lead to better monitoring and early detection.
Resources for Patient Screening
If you are already working as a mammographer, there are several trusted resources and websites for staying educated and having better conversations with your patients:
- DenseBreast-info.org®
- Are You Dense?®
- Find it Early Act
- FDA
- MQSA
- American College of Radiology
- American Cancer Society
Excel in Mammography With MTMI
In the heavily regulated business of mammography, it’s crucial to keep up with updates in the field. Failing to remain up to speed on the latest regulations and educational resources can not only be a detriment to the patients you serve, but it could also mean regulatory trouble for your facility at large.
That’s why MTMI is proud to provide quality training and multiple courses in mammography as it relates to breast cancer risk, breast imaging and screening, and more:
- Initial Mammography Course
- Breast Ultrasound Training Course
- Advanced Mammography Positioning
- MQSA Conquering Workflow Webinar
- Mammography Training for Technologists
MTMI programs are taught by experts with national reputations in their fields and cover many modalities. Our cross-training courses, offered in the classroom as well as via webinars, prepare you for registry exams and take your career to the next level. Check out our full catalog of programs or contact us with questions today!