Updated March 2023 – see new section, “2023 Study of DBT vs Digital Mammography”
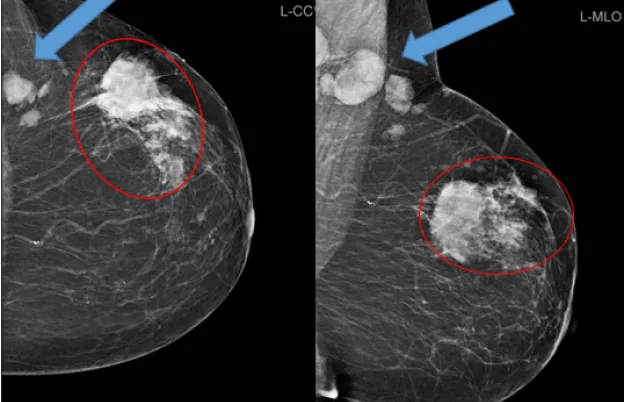
Digital Breast Tomosynthesis (DBT) is a three-dimensional technology that provides thin cross-sectional images through the breast. This technology is designed to prevent overlying structures from obscuring breast masses and prevent normal structures from being falsely identified as suspicious abnormalities.
In recent years, the demand for Digital Breast Tomosynthesis technology has grown, which has led to the belief that it’s new. While it may be the latest mammography modality approved by the Food and Drug Administration (FDA), the Hologic manufacturer released their Selenia Dimensions unit in 2011. The FDA has since approved three more manufacturers: GE, Siemens, and Fujifilm.
What Is Digital Breast Tomosynthesis?
Tomosynthesis is the process of taking multiple, high-resolution digital images of the breast at different angles. The angular ranges will vary from 15 degrees to 50 degrees depending on the manufacturer. There is a unique reconstruction algorithm that will take all the angled projections and convert them into thin 1 MM slices. The slices are then stacked on top of each other so the radiologist can scroll through them like turning pages in a book.
Is Tomosynthesis the same as 3D Mammography?
Tomosynthesis is synonymous with 3D mammography, allowing technologists to describe the imaging process to their patients in layman’s terms. The use of 3D mammography provides more information than 2D mammography alone. This means radiologists can more accurately detect breast cancer at earlier stages in addition to reducing the need for additional imaging.
Breast Tomosynthesis (3D) vs. 2D Mammography
Similar to how digital cameras took over film cameras, Digital mammography began replacing conventional film mammography with great strides around the year 2005. Two-dimensional (2D) mammograms are taken in one projection with the tube head at a 0 degrees angle from the imaging receptor. DBT or 3D mammography will use a direct or indirect digital image receptor and take 9 to 25 projections with the tube head at different angles. These projections are converted to thin, millimeter slices with software to create a 3D model with depth perception, allowing for more comprehensive image review with less structure overlap.
2023 Study of DBT vs Digital Mammography
After the initial publication of this blog in 2022, exciting new research was published in March of 2023 comparing the outcomes of women imaged with DBT and those imaged with Digital (2D) Mammography. This study found higher cancer detection rates and fewer call back rates with the use of 3D over 2D. 2D digital mammography is still standard at many sites, so this research was critical to improve patient outcomes and advance the standard of care towards Digital Breast Tomosynthesis. Over 1 million women were included who were imaged between January 2014 and December 2020 at 5 different large US health care systems. This research study, as well as others like it, may lead to wider adoption of Digital Breast Tomosynthesis, better cancer detection rates, and an increase in demand for mammographers who can use DBT.
Radiation Dose During Breast Tomosynthesis
Per FDA guidelines, radiation dosage in mammography must be kept very low, no more than 300 mrads or 3 mGy per view. Depending on the filter and anode material combination on a unit, a patient can expect an average of 1.2 mGy of radiation exposure for 2D mammography and 1.4-1.5 mGy for 3D mammography. When added together, this is below the 3 mGy limit and is lower than the dose given in film screen mammography. With today’s software advancements, the 2D image can be synthetically created from the 3D images, thus eliminating the 2D dose. According to Deborah Thames, MSRS, RT(R)(M)(QM), MTMI instructor & lead technologist at MD Anderson Cancer Center in Houston, Texas, another way of looking at it like this; a mammogram is the equivalent of background radiation you would be exposed to while walking around on the earth for two months.
3D Mammography Pros & Cons
As with any technology, there are benefits and drawbacks. Deborah Thames provides an insider’s perspective on some of the pros and cons of Digital Breast Tomosynthesis.
Pros
- 3D digital mammography separates superposed tissue into 1-2 millimeter slices, according to the unit’s technology. So, for example, if the breast is five centimeters thick, the software will provide the radiologist with 50 images. In conventional 2D mammography, those images would all be one with superimposed breast tissue, potentially hiding pathologies.
- With 3D mammography, the radiologist can more easily see within these individual slices and be assured there is nothing but normal tissue reducing false positive readings and reducing the need for unnecessary breast biopsies.
- The reduction in false positive readings means the recall rate for patients is lowered, reducing unnecessary patient anxiety.
- Edge depiction is improved with Digital Breast Tomosynthesis, meaning the radiologist can more often see a lesion as a whole and accurately measure it. Having accurate measurements of a malignant mass allows for accurate staging of breast cancer and correct treatment planning. Edge depiction also improves the radiologist’s ability to differentiate between benign mass characteristics and malignant mass characteristics.
- 3D mammography can help determine if additional breast imaging modalities such as ultrasound, MRI, or molecular breast imaging are warranted.
Cons
- All personnel involved, radiologists, medical physicists and mammography technologists are required to have 8 hours of DBT training.
- It can be challenging to adjust to detecting abnormalities in one-millimeter slices, especially calcification that can have different distributions in the breast which are now separated by the slices in the software.
- There are also more images for the radiologist to look at, meaning the reading process can be more time-consuming.
- One of the ways that abnormalities “pop” on mammography images is the brightness level, but the brightness of the images in 3D mammography is much lower than with 2D mammography. It can take a while for a radiologist to adjust to recognizing abnormalities accurately without this tell-tale brightness to grab their attention.
- Some DBT units, depending on the manufacturer, may require more space due to the angle that the tube moves.
- There are additional costs associated with DBT units, including facility accreditation, increased bandwidth requirements, and more quality control testing.
Cost of DBT
The cost associated with DBT units varies based on the age of the technology, manufacturer, and the service contracts facilities enter with the manufacturers. The price of the units can range from $85K - $275K, based on age and manufacturer. Further complicating the cost issue, the “best” mammography system differs for every facility, depending on factors such as practice goals, patient volume, and budgets.
One potentially prohibitive cost for some facilities isn’t even the DBT unit itself but the space in which the unit will be housed. As previously mentioned, DBT units need more space for the C arm that arcs from side to side over the patient. A major renovation will be necessary to accommodate the addition if a facility currently lacks the space for such a large machine.
To perform mammography in the United States, mammography facilities must be accredited every 3 years by an FDA approved accrediting body. Each facility is responsible for paying for these expenses. Deborah Thames’ facility has 17 units, and the cost of the first unit is $2700 for a unit that has 2 modes such as 3D mammography. For each additional unit that has 2 modes the cost is $2500. Along with the ACR, there are 2 states that are also FDA approved accreditation bodies, the states of Texas and Arkansas. Breast centers in those 2 states can choose if they want to use the ACR or their own state as their accrediting body. All other states in the United States must use the ACR. The ACR and 2 state accreditation bodies may have different costs associated with accreditation. In addition to ACR accreditation, all mammography breast centers in the United States need to pass an annual MQSA inspection to be certified for the next year. There are also costs associated with MQSA inspections that have to be paid.
After purchasing the unit, facilities also have to pay to keep the machines in working order, which can be quite costly. While an imaging center may enter into a service contract with their manufacturer, many facilities choose to have a field engineer on-site, especially in larger practices with multiple machines that could break down at any time. Mammography facilities must also employ a medical physicist to monitor the machines and conduct an annual medical physicist survey.
Why Radiologists, Technologists and Medical Physicists Need Digital Breast Tomosynthesis Training
Under the U.S. law called the Mammography Quality Standards Act (MQSA) all personnel must have 8 hours of training in Digital Breast Tomosynthesis (DBT) before they will be able to perform mammograms on 3D mammography machines, without supervision or dictate 3D mammography exams without supervision. Any breast center that has 3D mammography machines will need to have their staff complete this training. While the FDA’s Division of Mammography Quality Standards (DMQS) recognizes there are some features that are unique to each specific DBT system, personnel need only obtain training on one DBT system, or general DBT training, to meet the new modality training requirement. DBT technologists are encouraged to pursue additional training on their particular unit(s) to be as familiar as possible with their functionality.
Training is necessary for staff to properly understand the technology they are working with. They need to be able to maneuver the console screen commands, understand the theory of DBT, and learn the unique features of the facility’s unit.
How to Get DBT Certified
Mammographers can obtain their eight hours of DBT training for certification in various ways. The four manufacturers have training consultants who can train mammographers on their specific units.
There are also Continuing Education Instructors with DBT qualifications who can offer:
- In-person courses
- On-demand
- Peer-to-peer training by MQSA-certified technologists
Whatever form of training a mammographer, radiologist or medical pursues, the individual providing the training must be a qualified instructor, defined as an individual whose training and experience adequately prepare them to carry out specified training assignments. At the end of the training, personnel must be able to provide documentation demonstrating eight hours of training. Documentation may include:
- letters
- certificates
- documents from manufacturers or formal training courses
- confirming letter from a Continuing Education Unit granting organization
- attestation about experience.
MTMI Mammography Courses
Medical Technology Management Institute (MTMI) has several mammography training courses you can take to learn about Digital Breast Tomosynthesis. If you are a technologist just starting in the field, our initial mammography training course includes an optional 6th day devoted solely to DBT training. Alternatively, our single-day DBT training course is offered independently for those already familiar with mammography practice. For physicists, we offer a hands-on DBT training workshop.
MTMI programs are taught by experts with national reputations in their fields and cover every modality. Our cross-training courses are offered in the classroom and via webinars and prepare you for registry exams, accreditation, and to take your career to the next level. Check out our full catalog of programs, or contact us with questions today!













 at checkout.
at checkout.