Breast imaging plays a critical role in early breast cancer detection. These days, most women are well aware of the need for regular mammograms, with Centers for Disease Control data revealing that 69 percent of those over the age of 40 have done exactly that in the last two years. While most are willing to commit to these exams, many struggle to understand what their results mean.
This lack of clarity can extend into the medical profession, as breast imaging can be extremely nuanced. Hence the importance of assessment systems, which allow different members of the imaging team to communicate more effectively with each other and different teams.
BI-RADS® forms the basis of this communication, providing a framework through which healthcare professionals can share and analyze results. This, in turn, plays heavily into further testing, diagnosis, and, ultimately, treatment protocol. Below, we clarify the value of BI-RADS and break down its categories.
What Is BI-RADS? Why Is it Important?
The acronym BI-RADS stands for Breast Imaging Reporting and Data System. This term is a registered trademark of the American College of Radiology (ACR). MTMI's Miranda M. Lyman-Hager, RT(R)(M) refers to this acronym as a "name brand for assessment categories."
While not all facilities use BI-RADS as their assessment categories, all facilities must use assessment categories in their medical reports due to MQSA law. Mammography Quality Standards Act (MQSA) was an act passed by Congress in the ’90s to promote widespread high-quality mammography services in the United States.
MQSA serves many functions — such as ensuring that all mammography facilities are accredited and certified — one of its most noteworthy requirements involves the mandated use of assessment categories for breast imaging. Facilities that use the term BI-RADS have secured accreditation from ACR, which is one of the field's top accrediting bodies.
The vast majority of imaging centers currently use BI-RADS, but exceptions exist. Arkansas and Texas, for example, have state accreditation bodies. These state accreditation bodies require identical language to be used in the assessment categories within the medical records to meet MQSA standards.
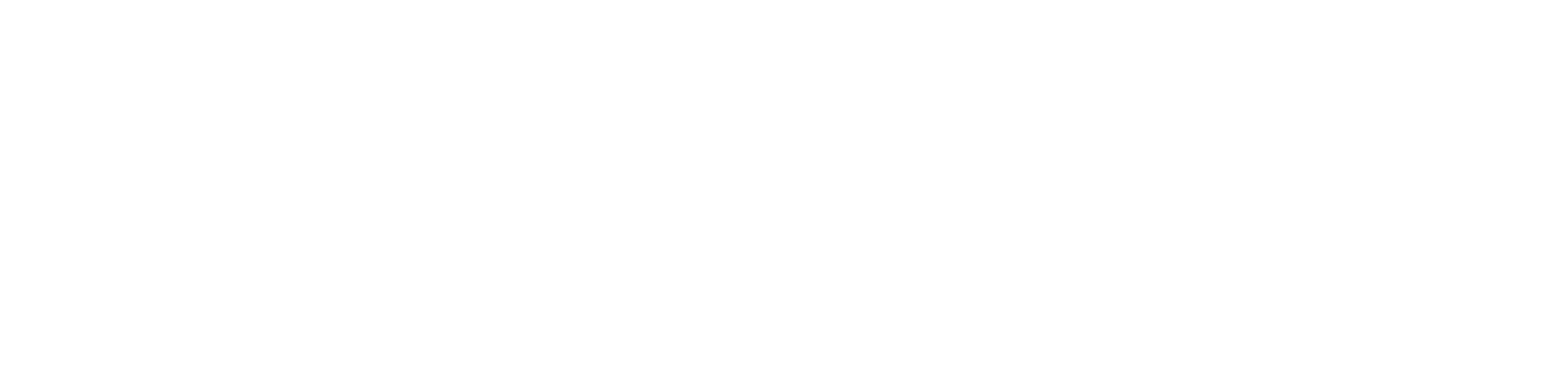
BI-RADS Categories
There are a total of seven numerical BI-RADS categories, each indicating the recommended management for the patient’s next steps in breast imaging. The most severe BI-RADS categories will rarely be assigned after a single mammogram. Instead, the radiologist will typically assign a category 0 so that more imaging can be done before eventually adjusting to whichever category is most relevant.
(table from ACR)
BI-RADS 0: Incomplete
Simply put, this category indicates that additional insight is required. The radiologist may be concerned that a mass or calcifications looks suspicious but would like more detailed imaging of it before deciding to recommend a biopsy. Or, if the patient has previously undergone imaging, comparisons with those prior images are being requested by the radiologist.
Once sufficient evidence is available to determine the presence of malignancy, benign masses, or no abnormalities, the radiologist can then shift the result to category 1-5.
BI-RADS 1: Negative
Also known in layman's terms as “normal.” Category 1 reveals that there are no abnormal calcifications or masses. The term “negative” suggests that nothing abnormal was found on this occasion and that, as a result, there is no further need for testing or biopsies at the moment. Lyman-Hager explains that this category is "reserved for those ladies who have mostly fat in the breast...there's nothing to see."
BI-RADS 2: Benign Finding
While category 2 technically constitutes a negative result (as there is no actual sign of cancer), it warrants a separate designation from the negative category highlighted above.
This result occurs when non-cancerous elements are discovered, such as a simple cyst or benign calcifications. Still, as Lyman-Hager clarifies, categories 1 and 2 should essentially be the same in the eyes of the patient. Benign findings are perfectly normal for many women, especially as they age — so category 2 should not be cause for alarm.
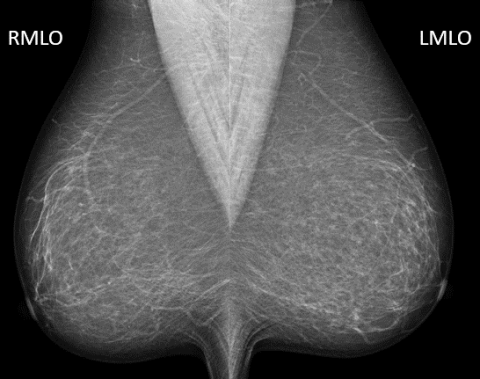
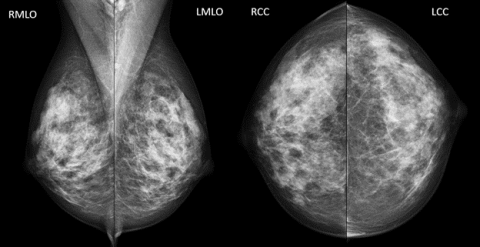
BI-RADS 3: Probably Benign
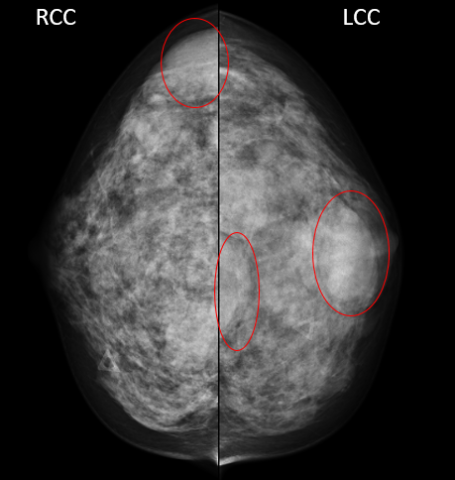
This mammogram shows several benign simple cysts in both breast (confirmed with an ultrasound exam). The radiologist recommended the patient return in 6 months for a follow up imaging to confirm stability of the cysts.
This category can feel like a gray area on the BI-RADS scale. The radiologist feels strongly that everything he or she sees is benign, but would like to be sure by checking it again in a short interval follow-up. To qualify for this category, suspicion must be extraordinarily low; nothing over 2 percent will make the cut.
Still, since it cannot technically be proven that the area is benign without a biopsy, follow-up imaging is recommended. This might mean additional imaging in six months or sometimes sooner.
Patients assigned this category will be told that their situation is most likely benign — but follow-up imaging should confirm that. Essentially, this is a "better safe than sorry" mentality, as early detection is a vital part of effective treatment.
BI-RADS 4: Suspicious Abnormality
The radiologist now feels that a biopsy is worthwhile. Lyman-Hager explains that this is when radiologists really start to feel suspicious.
This category covers a lot of ground, so it can be divided into three subcategories. These don't necessarily need to be referenced in official reports, but they can provide valuable insight into the individual circumstances at play.
BI-RADS 4a: Low Suspicion for Malignancy
If the likelihood of cancer falls somewhere between 2 and 10 percent, test results qualify as 4a.
BI-RADS 4b: Moderate Suspicion for Malignancy
Covering a wider range than category 4a, this designation involves a likelihood of anywhere between 10 and 50 percent.
BI-RADS 4c: High Suspicion for Malignancy
This designation involves a more than 50 percent chance, up to a 95 percent likelihood of cancer.
Next Steps
No matter which BI-RADS 4 subcategory is assigned, the next action will always be the same: a recommendation for a biopsy (tissue diagnosis). Lyman-Hager highlights the importance of this extra step, explaining, "At the end of the day, we need a biopsy because the only way to know for sure that this person has either a benign or malignant pathology is to take a tissue sample."
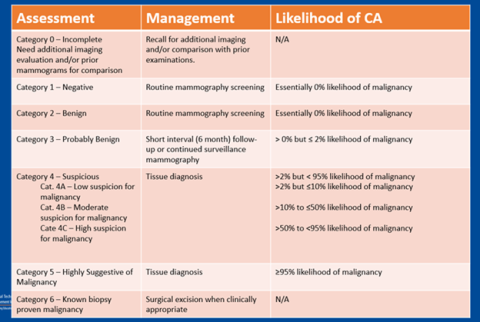
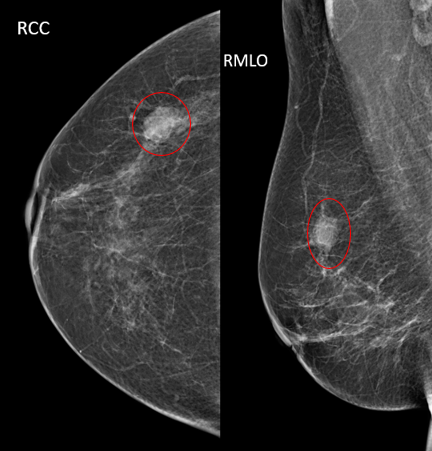
BI-RADS 5: Highly Suggestive of Malignancy
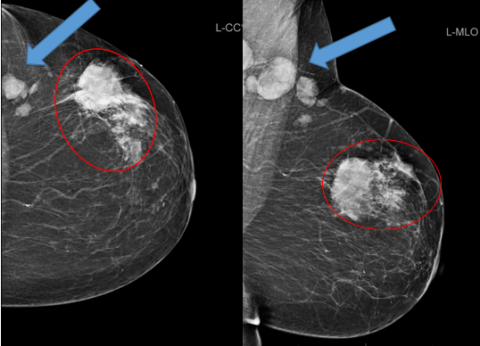
Highly suspicious mass (circle) with abnormal looking lymph nodes (arrow).
This designation indicates that, based on imaging results, there is a 95 percent chance of cancer. Biopsy (tissue diagnosis) is strongly recommended. Lyman-Hager explains, "In the eyes of the radiologist, this is what cancer looks like on an image."
BI-RADS 6: Known Biopsy-Proven Malignancy
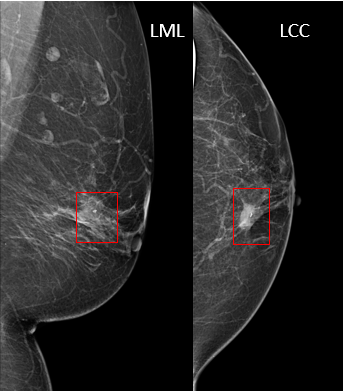
This mammogram shows where the localization seed was placed that will lead the surgeon to the tissue that needs to be removed.
This category is only used if previous biopsies have revealed that cancer is present. In this situation, certain imaging can provide valuable insight for surgical excision; these imaging studies are given a BI-RADS 6.
BI-RADS Modalities
BI-RADS assessment categories are used in all breast imaging modalities which include:
Mammography
As the gold standing in the fight against breast cancer, mammography is a tool used for women annually. Mammography functions a lot like a revolving door; patients continue to get recommendations and return for routine annual “screening” mammography.
The main purpose of this modality is early detection. Mammograms are excellent for revealing microcalcifications, which can be the earliest sign of breast cancer.
Ultrasound
Often, mammography is complemented by ultrasounds, which are particularly useful when patients have dense breast tissue. Similarly, this modality can be helpful when radiologists struggle to determine whether masses are solid or fluid filled.
MRI
Another modality ideal for examining patients with dense breast tissue or breast implants, magnetic resonance imaging (MRI) often steps in for surgical navigation purposes once a possible malignancy has been detected. This can help determine whether vascular attachments exist, as these could have a huge impact on future treatment options. Otherwise, MRIs also serve as a valuable secondary screening tool for high-risk patients.
Patients and BI-RADS
BI-RADS assessment categories communicate information to physicians, but it is not meant to frame discussions with patients. Instead, BI-RADS results are interpreted and then conveyed to patients in a way that they can better understand through a lay letter. For example: if a patient is assessed as category 0, she will simply be told that comparison images are required and or that additional imaging is being recommended to complete her study.
It is not the role of the breast imaging technologist to interpret, diagnose, or discuss results with patients. That said, if a patient is aware of their BI-RADS category from a results summary or online health portal, a technologist can help them understand the strict definition of that assessment category and how it is used.
Future Changes to BI-RADS
BI-RADS categories have dominated breast imaging procedures and test interpretation for years — and that's not about to change. If anything, BI-RADS will become even more dominant in years to come. The FDA announced on March 9, 2023, that by September 10, 2024, all 50 states will be required to include standardized communication about breast tissue density. Facilities must begin separating all patients into categories ‘non-dense’ (BI-RADS A or B) or ‘dense’ (BI-RADS C or D) with specific communication depending on category.
Additional changes will be prompted by evolving technologies and research-backed solutions.
Learn More About Mammography and Breast Imaging
If you're passionate about mammography and eager to make a difference through early breast cancer detection, you could be an excellent candidate for a rewarding career in mammography. First, however, you'll need targeted training. After you become an x-ray tech, training includes initial mammography technologist training. Additionally, if you are planning to sit for the ARRT certification exam soon, our mammography registry review provides a live instructor-led interactive program giving you what you need to prepare for the test.
Already a mammographer? You can elevate your skills at our Advanced Mammography Positioning Course. Designed for any level mammographer, this hands-on program covers positioning patients with implants, wheelchair patients, kyphotic patients and other special circumstances. You may also want to consider expanding your knowledge by becoming a breast sonographer with our breast ultrasound course.
MTMI programs are taught by experts with national reputations in their fields and cover many modalities. Our cross-training courses, offered in the classroom as well as via webinars, prepare you for registry exams and take your career to the next level. Check out our full catalog of programs, or contact us with questions today!